In 1976, beloved chef, cookbook author and television personality Julia Child returned to WGBH-TV’s studios in Boston for a new cooking show, “Julia Child & Company,” following her hit series “The French Chef.”
Viewers probably didn’t know that Child’s new and improved kitchen studio, outfitted with gas stoves, was paid for by the American Gas Association.
While this may seem like any corporate sponsorship, we now know it was a part of a calculated campaign by gas industry executives to increase use of gas stoves across the United States.
And stoves weren’t the only objective. The gas industry wanted to grow its residential market, and homes that used gas for cooking were likely also to use it for heat and hot water.
The industry’s efforts went well beyond careful product placement, according to new research from the nonprofit Climate Investigations Center, which analyzes corporate efforts to undermine climate science and slow the ongoing transition away from fossil fuels.
As the center’s study and a National Public Radio investigation show, when evidence emerged in the early 1970s about the health effects of indoor nitrogen dioxide exposure from gas stove use, the American Gas Association launched a campaign designed to manufacture doubt about the existing science.
As a researcher who has studied air pollution for many years – including gas stoves’ contribution to indoor air pollution and health effects – I am not naïve about the strategies that some industries use to avoid or delay regulations.
But I was surprised to learn that the multipronged strategy related to gas stoves directly mirrored tactics that the tobacco industry used to undermine and distort scientific evidence of health risks associated with smoking starting in the 1950s.
Manufacturing controversy
The gas industry relied on Hill & Knowlton, the same public relations company that masterminded the tobacco industry’s playbook for responding to research linking smoking to lung cancer.
Hill & Knowlton’s tactics included sponsoring research that would counter findings about gas stoves published in the scientific literature, emphasizing uncertainty in these findings to construct artificial controversy and engaging in aggressive public relations efforts.
For example, the gas industry obtained and reanalyzed the data from an EPA study on Long Island that showed more respiratory problems in homes with gas stoves. Their reanalysis concluded that there were no significant differences in respiratory outcomes.
The industry also funded its own health studies in the early 1970s, which confirmed large differences in nitrogen dioxide exposures but did not show significant differences in respiratory outcomes.
These findings were documented in publications where industry funding was not disclosed. These conclusions were amplified in numerous meetings and conferences and ultimately influenced major governmental reports summarizing the state of the literature.
This campaign was remarkable, since the basics of how gas stoves affected indoor air pollution and respiratory health were straightforward and well established at the time.
Burning fuel, including natural gas, generates nitrogen oxides: The air in Earth’s atmosphere is about 78% nitrogen and 21% oxygen, and these gases react at high temperatures.
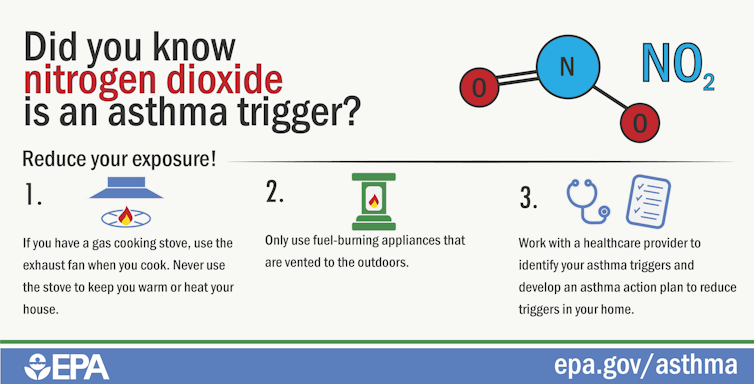
Nitrogen dioxide is known to adversely affect respiratory health. Inhaling it causes respiratory irritation and can worsen diseases such as asthma. This is a key reason why the U.S. Environmental Protection Agency established an outdoor air quality standard for nitrogen dioxide in 1971.
No such standards exist for indoor air, but as the EPA now acknowledges, nitrogen dioxide exposure indoors also is harmful.
How harmful is indoor exposure?
The key question is whether nitrogen dioxide exposure related to gas stoves is large enough to lead to health concerns. While levels vary across homes, scientific research shows that the simple answer is yes – especially in smaller homes and when ventilation is inadequate.
This has been known for a long time. For example, a 1998 study that I co-authored showed that the presence of gas stoves was the strongest predictor of personal exposure to nitrogen dioxide.
And work dating back to the 1970s showed that indoor nitrogen dioxide levels in the presence of gas stoves could be far higher than outdoor levels. Depending on ventilation levels, concentrations could reach levels known to contribute to health risks.
Despite this evidence, the gas industry’s campaign was largely successful. Industry-funded studies successfully muddied the waters, as I have seen over the course of my research career, and stalled further federal investigations or regulations addressing gas stove safety.
This issue took on new life at the end of 2022, when researchers published a new study estimating that 12.7% of U.S. cases of childhood asthma – about one case in eight – were attributable to gas stoves. The industry continues to cast doubt on gas stoves’ contribution to health effects and fund pro-gas stove media campaigns.
A concern for climate and health
Residential gas use is also controversial today because it slows the ongoing shift toward renewable energy, at a time when the impacts of climate change are becoming alarmingly clear. Some cities have already moved or are considering steps to ban gas stoves in new construction and shift toward electrifying buildings.
As communities wrestle with these questions, regulators, politicians and consumers need accurate information about the risks of gas stoves and other products in homes. There is room for vigorous debate that considers a range of evidence, but I believe that everyone has a right to know where that evidence comes from.
The commercial interests of many industries, including alcohol, tobacco and fossil fuels, aren’t always compatible with the public interest or human health. In my view, exposing the tactics that vested interests use to manipulate the public can make consumers and regulators savvier and help deter other industries from using their playbook.![]()
Jonathan Levy, Professor and Chair, Department of Environmental Health, Boston University
This article is republished from The Conversation under a Creative Commons license. Read the original article.







